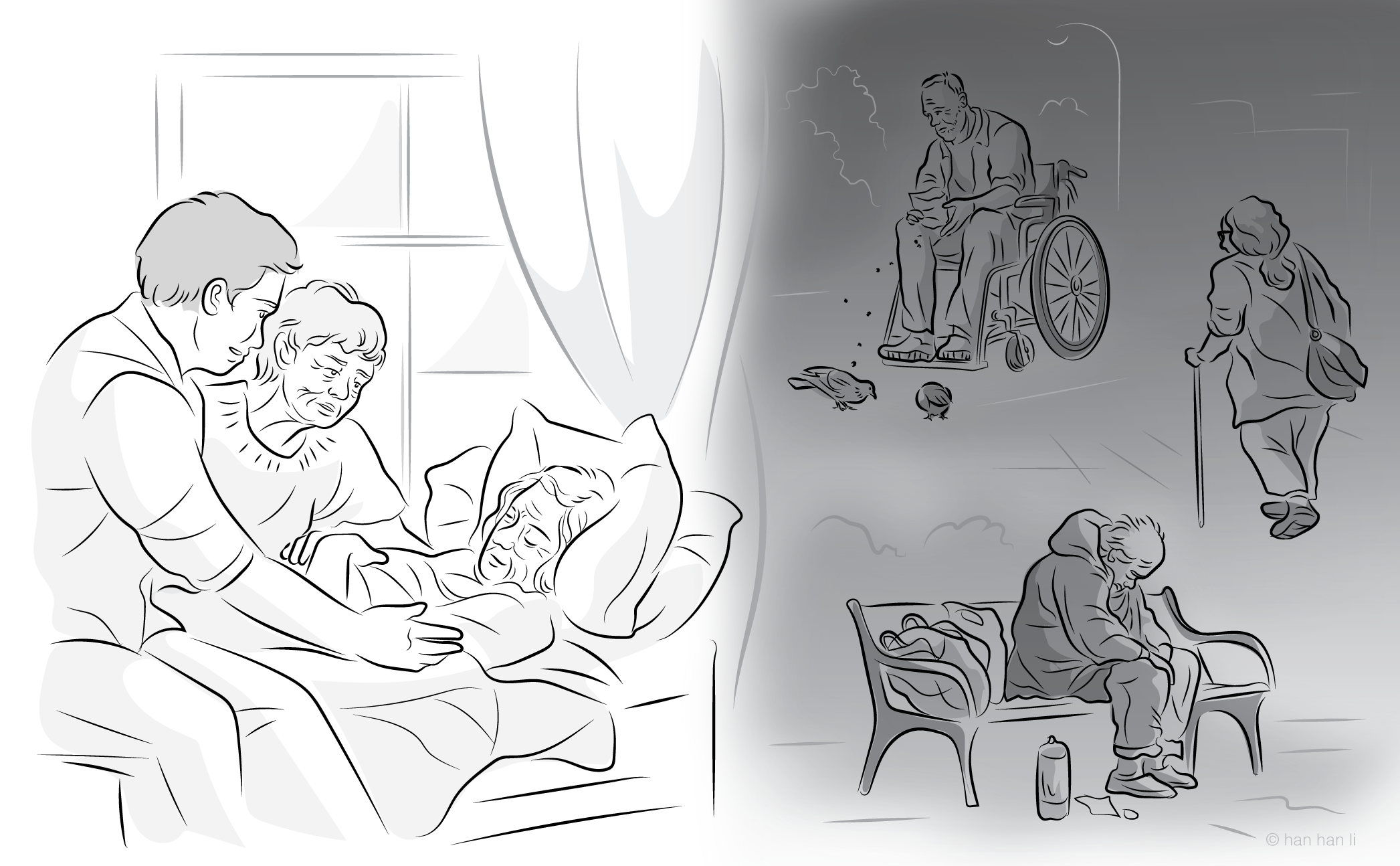
MAiD, Mental Disorder, and Capacity: Recognizing the Complexity of Moral Agency in Capacity Assessment
DOI:
https://doi.org/10.7202/1121336arKeywords:
MAiD, MD-SUMC, moral agency, decision-making capacity, consent, mental disorder, valuesLanguage(s):
EnglishAbstract
Medical assistance in dying (MAiD) has become a prominent form of end-of-life care within the Canadian health system, yet it is not without its critics. Drawing even more critical attention is the possibility of Canada expanding MAiD eligibility to persons who suffer from mental disorder as their sole underlying medical condition (MAiD MD-SUMC). Unlike physical conditions that cause pain and suffering, mental disorder has the intrinsic potential to affect one’s ability to understand and appropriately value the consequences of one’s actions and decisions. There is thus a significant risk that a patient who has requested MAiD MD-SUMC may be unable to provide valid consent due to an impaired ability to either: 1) adequately understand the consequences of receiving MAiD or 2) place that consequence within a consistent set of values. Due to the important ways in which mental disorder can affect one’s values and desires, this paper argues that we must evaluate decision-making capacity in a more holistic way that includes both cognitive and evaluative factors. My argument is based upon a presentation of the evaluative factors involved in decision-making, a demonstration that these factors may be significantly affected by mental illness, and a suggestion that we require more holistic criteria for capacity evaluation than the excessively cognitive criteria espoused by most commonly used assessment tools. Because of the interplay between these aspects of my argument and the extremely high stakes involved in MAiD assessments, I suggest that capacity evaluations (both in general and especially for MAiD requests) ought to incorporate an aspect of narrative assessment by which the patient’s values and self-understanding can be better assessed.
References
1. Department of Justice Canada. Canada’s Medical Assistance in Dying (MAID) Law. Ottawa: Government of Canada. 31 Jul 2024
2. Zhong R, Xu Y, Oquendo MA, Sisti DA. Physician aid-in-dying for individuals with serious mental illness: clarifying decision-making capacity and psychiatric futility. American Journal of Bioethics. 2019;19(10):61-3.
3. Kontos N, Freudenreich O, Querques J. “Poor insight”: a capacity perspective on treatment refusal in serious mental illness. Psychiatric Services. 2016;67(11):1254-6.
4. Cohen J, Van Landeghem P, Carpentier N, Deliens L. Public acceptance of euthanasia in Europe: a survey study in 47 countries. International Journal of Public Health. 2014;59(1):143-56.
5. Appelbaum PS. Physician-assisted death for patients with mental disorders—reasons for concern. JAMA psychiatry. 2016;73(4):325-6.
6. Kim SYH, De Vries RG, Peteet JR. Euthanasia and assisted suicide of patients with psychiatric disorders in the Netherlands 2011 to 2014. 2016;73(4):362-8.
7. Olié E, Courtet P. The controversial issue of euthanasia in patients with psychiatric illness. JAMA. 2016;316(6):656-7.
8. Price A, McCormack R, Wiseman T, Hotopf M. Concepts of mental capacity for patients requesting assisted suicide: a qualitative analysis of expert evidence presented to the Commission on Assisted Dying. BMC Medical Ethics. 2014;15:32.
9. Sumner LW. Assisted Death: A Study in Ethics and Law. Oxford: Oxford University Press; 2011.
10. Doorn N. Mental competence or capacity to form a will: an anthropological approach. Philosophy, Psychiatry & Psychology. 2011;18(2):135-45.
11. O’Neill O. Autonomy and Trust in Bioethics. 1st ed. Cambridge: Cambridge University Press; 2002.
12. Manson NC, O’Neill O. Rethinking Informed Consent in Bioethics. 1st ed. Cambridge: Cambridge University Press; 2007.
13. Jonsen AR. The Birth of Bioethics. New York: Oxford University Press; 1998.
14. Craigie J. Capacity, value neutrality and the ability to consider the future. International Journal of Law in Context. 2013;9(1):4-19.
15. Dworkin R. Life’s Dominion: An Argument about Abortion, Euthanasia, and Individual Freedom. 1st ed. New York: Vintage Books; 1994.
16. Lillehammer H. Autonomy, value, and the first person. In: Radoilska L, editor. Autonomy and Mental Disorder. New York: Oxford University Press; 2012. p. 192-214.
17. Bortolotti L, Cox R, Broome M, Mameli M. Rationality and self-knowledge in delusion and confabulation: implications for autonomy as self-governance. In: Radoilska L, editor. Autonomy and Mental Disorder. New York: Oxford University Press; 2012. p. 100-22.
18. Baker LR. Persons and Bodies: A Constitution View. Cambridge: Cambridge University Press; 2012.
19. Buchanan AE, Brock DW. Deciding for Others: The Ethics of Surrogate Decision Making. Cambridge: Cambridge University Press; 2012.
20. Arenella P. Character, choice and moral agency: the relevance of character to our moral culpability judgments. Social Philosophy & Policy. 1990;7(2):59-83.
21. Banner NF. Can procedural and substantive elements of decision-making be reconciled in assessments of mental capacity? International Journal of Law in Context. 2013;9(1):71-86.
22. Kious BM. Autonomy and values: why the conventional theory of autonomy is not value-neutral. Philosophy, Psychiatry & Psychology. 2015;22(1):1-12.
23. Spike JP. The differing role of narrative unity in the concepts of capacity versus competence. AJOB neuroscience. 2020;11(1):20-3.
24. Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 8th edition. New York: Oxford University Press; 2019.
25. Freeland A, Godkin D, Dembo J, et al. Medical assistance in dying (MAiD) for persons whose sole underlying medical condition is a mental disorder: challenges and considerations. Canadian Journal of Psychiatry. 2022;67(1):71-87.
26. Kim SYH. Canadian medical assistance in dying and the hegemony of privilege. American Journal of Bioethics. 2023;23(11):1-6.
27. Jones C, Draper B, Peisah C, Wand APF, Brodaty H. Rational suicide, euthanasia, and the very old: two case reports. Case reports in psychiatry. 2016;2016:4242064.
28. Olié E, Catanzaro T, Malestroit M, Guija JA, Giner L, Courtet P. The capacity to consent to treatment is altered in suicidal patients. Annals of General Psychiatry. 2023;22(1):35.
29. Wang YY, Wang SB, Ungvari GS, Yu X, Ng CH, Xiang YT. The assessment of decision‐making competence in patients with depression using the MacArthur competence assessment tools: A systematic review. Perspectives in Psychiatric Care. 2018;54(2):206-11.
30. Sangroula D, Mainali P, Hagi K, Peteru S. Psychiatric illness and medical decision-making capacity: a retrospective study in medical settings. Psychiatry International. 2020;1(2):115-24.
31. Banner NF. Can procedural and substantive elements of decision-making be reconciled in assessments of mental capacity? International Journal of Law in Context. 2013;9(1):71-86.
32. Hindmarch T, Hotopf M, Owen GS. Depression and decision-making capacity for treatment or research: a systematic review. BMC Medical Ethics. 2013;14:54.
33. Craine P. Questioning the ethics of assisted dying for the mentally ill. Canadian Journal of Bioethics / Revue Canadienne de Bioéthique. 2023;6(3-4):115-27.
34. Baruth JM, Lapid MI. Influence of psychiatric symptoms on decisional capacity in treatment refusal. AMA Journal of Ethics. 2017;19(5):416-25.
35. Grisso T. Assessing Competence to Consent to Treatment: A Guide for Physicians and Other Health Professionals. New York: Oxford University Press; 1998.
36. Craigie J. Competence, practical rationality and what a patient values. Bioethics. 2011;25(6):326-33.
37. Owen GS, Martin W, Gergel T. Misevaluating the future: affective disorder and decision-making capacity for treatment – a temporal understanding. Psychopathology. 2018;51(6):371-9.
38. Council of Canadian Academies. Medical Assistance in Dying: The Expert Panel on Medical Assistance in Dying. CCA Reports. 12 Dec 2018.
39. Goldberg AL. How bioethics and case law diverge in assessments of mental capacity: an argument for a narrative coherence standard. AJOB neuroscience. 2020;11(1):7-17.
40. Bratman M. Structures of agency: essays. Oxford ; Oxford University Press; 2007.
41. Rawls J. Political liberalism. Expanded edition. New York: Columbia University Press; 2005.
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Kyle J. Barbour

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Canadian Journal of Bioethics applies the Creative Commons Attribution 4.0 International License to all its publications. Authors therefore retain copyright of their publication, e.g., they can reuse their publication, link to it on their home page or institutional website, deposit a PDF in a public repository. However, the authors allow anyone to download, reuse, reprint, distribute, and/or copy their publication, so long as the original authors and source are cited.














_smaller.png)