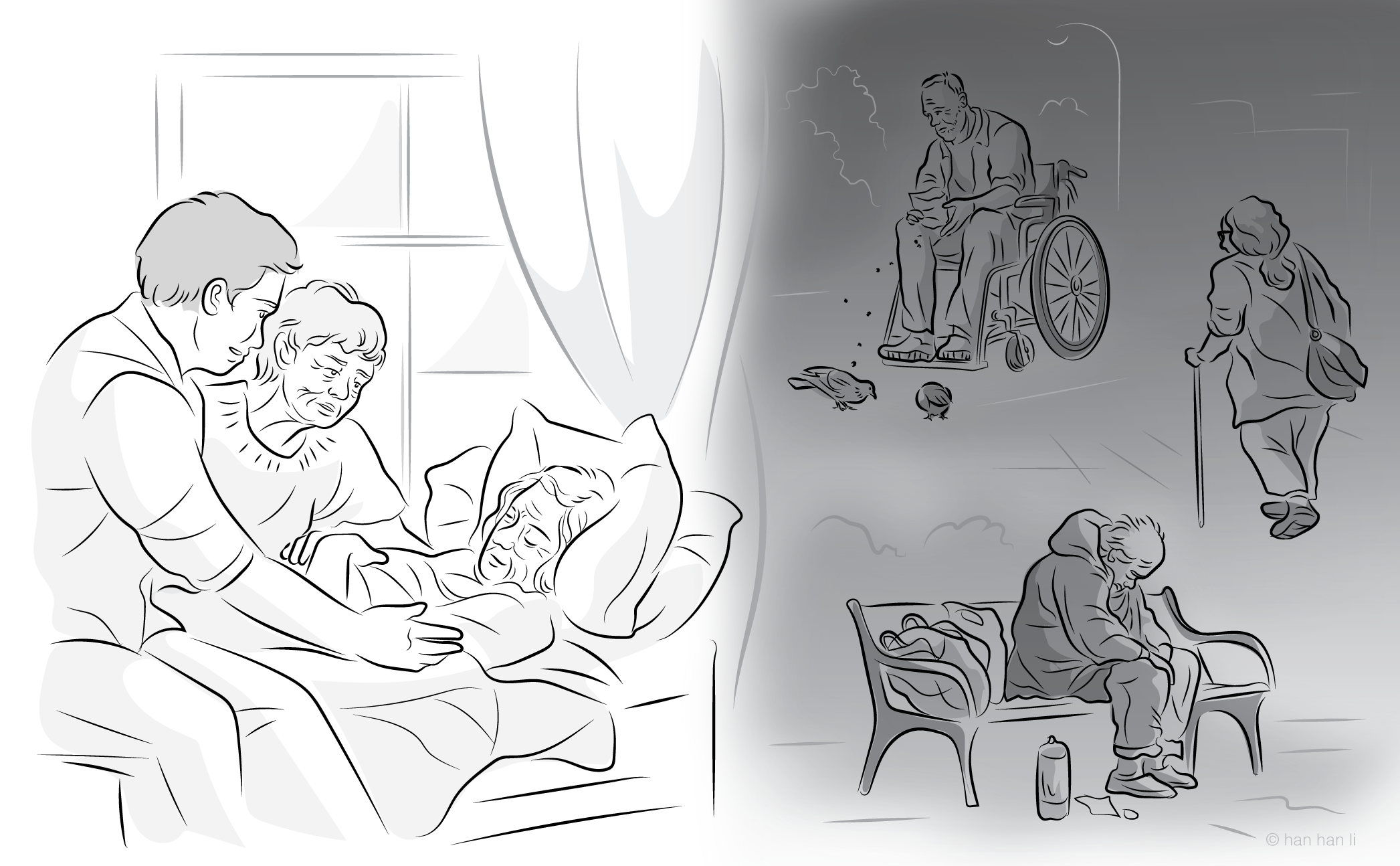
MAiD, Mental Disorders, and Vulnerability: How Common Responses to Vulnerability Concerns are Inadequate
DOI:
https://doi.org/10.7202/1121335arKeywords:
medical assistance in dying, MAiD, vulnerability, mental disorders, criteria, expansion, social sources of riskLanguage(s):
EnglishAbstract
The concept of vulnerability is bandied about frequently in ongoing debates about medical assistance in dying (MAiD) and who should be eligible, but is often used as a broad catch-all phrase to capture some sort of risk or concern that people have. This imprecise usage obfuscates the concerns that opponents to MAiD have about expansion to include those suffering from mental disorders as the sole underlying condition. Since what is intended to be captured by the term ‘vulnerable’ is at times unclear, attempts to respond to or mitigate this vulnerability can miss the mark. Arguments from vulnerability against expanding access to MAiD point out social and/or systemic factors that may influence the choices of people living with mental disorders to access MAiD, such as lack of access to adequate care, stigma and discrimination, suicidality, and the correlation between mental disorders and low socio-economic status. However, the common response to concerns about vulnerability, made by those who argue for expansion, focus on highlighting current safeguards that are in place to ensure only those who are eligible for MAiD gain access. Under this view, vulnerability is determined by assessing individuals for eligibility. Those who cannot meet the eligibility criteria would not be permitted access. Yet, this entirely misses the concerns being raised that point to systemic or social sources of risk. Ensuring that the individuals who access MAiD meet the criteria is to ignore the reasons for accessing it in the first place.
References
1. Tanner R. An ethical-legal analysis of medical assistance in dying for those with mental illness. Alberta Law Rev. 2018;56(1):149-75.
2. Rooney W, Schuklenk U, van de Vathorst S. Are concerns about irremediableness, vulnerability, or competence sufficient to justify excluding all psychiatric patients from medical aid in dying? Health Care Anal. 2018;26(4):326-43.
3. Blikshavn T, Husum TL, Magelssen M. Four reasons why assisted dying should not be offered for depression. J Bioethical Inq. 2017;14(1):151-57.
4. Kim SYH, Lemmens T. Should assisted dying for psychiatric disorders be legalized in Canada? CMAJ. 2016;188(14):E337-39.
5. Expert Panel on MAiD and Mental Illness. Final Report of the Expert Panel on MAiD and Mental Illness. Ottawa: Health Canada.
6. Lazin SJ, Chandler JA. Two views of vulnerability in the evolution of Canada’s Medical Assistance in Dying Law. Camb Q Healthc Ethics. 2023;32(1):105-17.
7. Mackenzie C, Rogers W, Dodds S, editors. Vulnerability: New Essays in Ethics and Feminist Philosophy. Oxford: Oxford University Press; 2014.
8. Rogers W, Mackenzie C, Dodds S. Why bioethics needs a concept of vulnerability. Int J Feminist Approaches Bioeth. 2012;5(2):11-38.
9. Rodriguez v. British Columbia (Attorney General). 1993 3 SCR 519.
10. Carter v. Canada (Attorney General). 2015 1 SCR 331.
11. Department of Justice. Legislative Background: Medical Assistance in Dying (Bill C-14). Ottawa: Government of Canada. 17 Jun 2016.
12. Truchon c. Procureur général du Canada. 2019 QCCS 3792.
13. House of Commons. Bill C-7. An Act to Amend the Criminal Code (Medical Assistance in Dying). Ottawa: Parliament of Canada; 2021.
14. Special Joint Committee Medical Assistance in Dying. MAID and Mental Disorders: The Road Ahead. Report of the Special Joint Committee; No. 3 - AMAD (44-1). Ottawa: Parliament of Canada.
15. Farrugia A, Penrod J, Bult JM. Payment, compensation and replacement—the ethics and motivation of blood and plasma donation. Vox Sang. 2010;99(3):202-11.
16. Health Canada. Model Practice Standard for Medical Assistance in Dying. Ottawa; Mar 2023.
17. Senate of Canada. Subject Matter of Bill C-7: An Act to Amend the Criminal Code (Medical Assistance in Dying). Report of the Standing Senate Committee on Legal and Constitutional Affairs. Ottawa: Senate; 2 Feb 2021.
18. Institute for Research and Development on Inclusion and Society. Bill C:7 Through a Disability Lens. Submission to the House of Commons Standing Committee on Justice and Human Rights. Ottawa; Nov 2020.
19. Council of Canadians with Disabilities. Brief of the Council of Canadians With Disabilities to the Standing Committee on Justice and Human Rights regarding Bill C-7, An Act to amend the Criminal Code (Medical Assistance in Dying). Ottawa; 31 Oct 2020.
20. Moroz N, Moroz I, Slovinec D’Angelo M. Mental health services in Canada: Barriers and cost-effective solutions to increase access. Healthc Manage Forum. 2020;33(6):282-87.
21. Coelho R. Disability and MAiD. In: Coelho R, Gaind KS, Lemmens T, editors. Unravelling MAiD in Canada: Euthanasia and Assisted Suicide as Medical Care. Montreal: McGill-Queen’s University Press; 2025. p.188-203.
22. Lyon CJ, Lemmens T, Kim SYH. Canadian medical assistance in dying: provider concentration, policy capture, and need for reform. Am J Bioeth. 2025;25(5):6-25.
23. Appelbaum PS. Should mental disorders be a basis for physician-assisted death? Psychiatr Serv. 2017;68(4):315-17.
24. Ho A, Norman JS. Social determinants of mental health and physician aid-in-dying: The real moral crisis. Am J Bioeth. 2019;19(10):52-4.
25. Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16-20.
26. Zamorano S, González-Sanguino C, Muñoz M. Implications of stigma towards mental health problems on suicide risk in people with mental health problems: a systematic review. Actas Esp Psiquiatr. 2022;50(5):216-25.
27. Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. 2014;15(2):37-70.
28. Fox AB, Earnshaw VA, Taverna EC, Vogt D. Conceptualizing and measuring mental illness stigma: The mental illness stigma framework and critical review of measures. Stigma Health. 2018;3(4):348-76.
29. Vulnerability and Social Policy Network. Why Vulnerability Matters. 2017.
30. Vulnerability and Social Policy Network. Understanding the Vulnerable Persons Standard. 2017.
31. Baril A. Undoing Suicidism: A Trans, Queer, Crip Approach to Rethinking (Assisted) Suicide. 1st ed. Temple University Press; 2023.
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Loughran Butcher

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Canadian Journal of Bioethics applies the Creative Commons Attribution 4.0 International License to all its publications. Authors therefore retain copyright of their publication, e.g., they can reuse their publication, link to it on their home page or institutional website, deposit a PDF in a public repository. However, the authors allow anyone to download, reuse, reprint, distribute, and/or copy their publication, so long as the original authors and source are cited.














_smaller.png)