The Moral Permissibility of Providing Medical Assistance in Dying in Canada: An Ethical Framework for Professional Practice
DOI:
https://doi.org/10.7202/1121333arKeywords:
medical assistance in dying, MAiD, voluntary euthanasia, assisted suicide, fiduciary duties, cruel choice, claim rights, privilege rightsLanguage(s):
EnglishAbstract
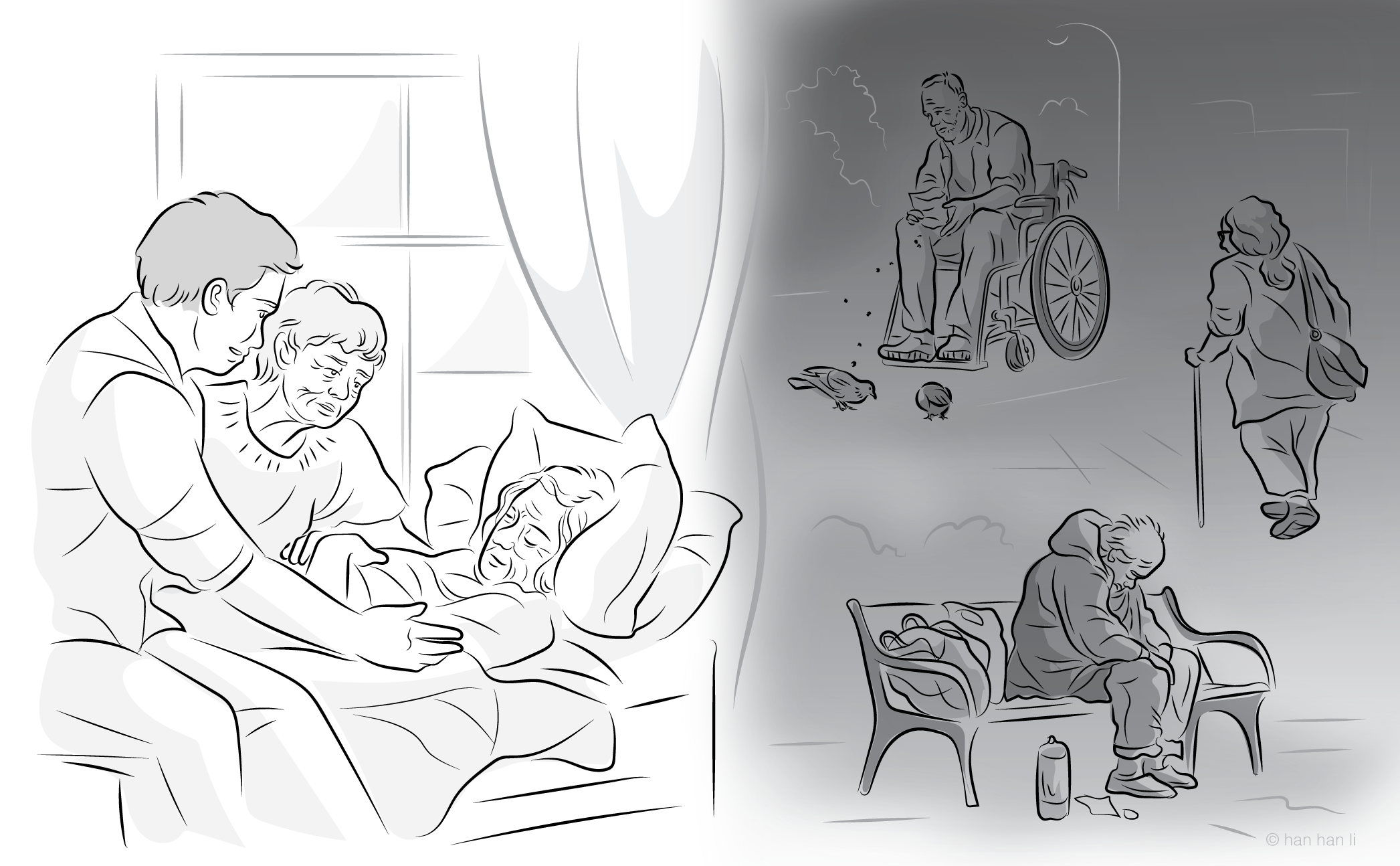
Although medical assistance in dying (MAiD) is legally permitted in Canada under defined statutory conditions, this legal framework does not determine when it is morally permissible for a healthcare professional to provide MAiD. This paper explicitly examines the normative distinction between legal and ethical MAiD practice. It argues that the medically related eligibility criteria, such as incurability, irreversible decline, and intolerable suffering, do not function as objective medical criteria but instead presuppose and reinforce patient autonomy. As a result, MAiD assessments are often reduced to procedural confirmations of autonomy rather than substantive medical assessments. Thus, autonomy has become the de facto justification for the provision of MAiD, even though Canadian law does not regard autonomy alone as a sufficient condition.
This paper examines the discretionary structure of MAiD practice and demonstrates that every decision to provide MAiD involves a normative judgment on the part of the healthcare professional. To guide that judgment, an ethics framework grounded in the fiduciary duties of healthcare professionals is proposed. Using the four core principles of healthcare ethics, this framework holds that it is morally permissible for a healthcare professional to provide MAiD only when: 1) the patient is autonomous, understood in terms of capacity, voluntariness, and informed consent; 2) the intervention satisfies the principles of beneficence and nonmaleficence; and 3) the request arises from a context of justice, in which a medical condition renders the patient unable to act on their autonomous wish to die without assistance.
References
1. Carter v Canada (Attorney General), 2015 SCC 5, [2015] 1 SCR 331 at para 105.
2. Lyon C, Lemmens T, Kim SYH. Canadian medical assistance in dying: provider concentration, policy capture, and need for reform. Am J Bioeth. 2025;25(5):6-25.
3. Health Canada. Fifth Annual Report on Medical Assistance in Dying in Canada. Ottawa; 11 Dec 2024.
4. Close E, Downie J, White BP. Practitioners’ experiences with 2021 amendments to Canada’s medical assistance in dying law: a qualitative analysis. Palliat Care Soc Pract. 2023;17:26323524231218282.
5. Medical Assistance in Dying. Criminal Code, RSC 1985, c C-46, s 241.1.
6. Law Reform Commission of Canada. Euthanasia, aiding suicide and cessation of treatment. Working Paper 28. Ottawa; 1983.
7. Law Reform Commission of Canada. Report 20: Euthanasia, Aiding Suicide and Cessation of Treatment. Ottawa; 1983.
8. Keyserlingk EW. Assisted suicide, causality and the Supreme Court of Canada. McGill Law J. 1994;39(2):285-328.
9. Senate of Canada. Of Life and Death - Final Report. Special Senate Committee on Euthanasia and Assisted Suicide, 35th Parliament, 1st Session. Ottawa; 1994.
10. Elsner AM, Frank CE, Keller M, McCullough JO, Rampton V. Language matters: the semantics and politics of “assisted dying”. Hastings Cent Rep. 2024;54(5):3-7.
11. Collège des médecins du Québec. Physicians, appropriate care and the debate on euthanasia: a reflection. Montréal; 2 Nov 2009.
12. Commission spéciale sur la question de mourir dans la dignité. Mourir dans la dignité: rapport de la Commission spéciale sur la question de mourir dans la dignité. Québec: Assemblée nationale du Québec; 2012.
13. Assemblée nationale du Québec. Bill 52, An Act respecting end-of-life care, 2014, c 2. Québec: Gouvernement du Québec; 2014.
14. Gromadzki R, Christie T. Assisted suicide and euthanasia: language lost in MAiD. Can J Bioeth. 2024;7(2-3):159-65.
15. Government of Canada. An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying), SC 2016, c 3 (Bill C-14).
16. Government of Canada. An Act to amend the Criminal Code (medical assistance in dying), SC 2021, c 2 (Bill C-7).
17. Government of Canada. Criminal Code, RSC 1985, c C‑46, ss. 241.2 (as amended by SC 2016, c 3; SC 2021, c 2).
18. Parliament of Canada. How a bill becomes law. Ottawa; 2021.
19. Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 8th ed. New York: Oxford University Press; 2019.
20. Ross WD. The Right and the Good. Oxford: Clarendon Press; 1930/2002.
21. Truth and Reconciliation Commission of Canada. Honouring the Truth, Reconciling for the Future: Summary of the Final Report of the Truth and Reconciliation Commission of Canada. Ottawa; 2015.
22. Government of Canada. Interpretation Act, RSC 1985, c I‑21, s 11. Ottawa; 1985(rev 2025).
23. de Haan J. The ethics of euthanasia: advocates’ perspectives. Bioethics. 2002;16(2):154-72.
24. Sumner LW. Physician-Assisted Death: What Everyone Needs to Know. New York: Oxford University Press; 2017.
25. Davis J, Mathison E. The case for an autonomy‑centered view of physician‑assisted death. J Bioeth Inq. 2020;17(3):345-56.
26. Braun E. An autonomy-based approach to assisted suicide: a way to avoid the expressivist objection against assisted dying laws. J Med Ethics. 2023;49(7):497-501.
27. Germany. Judgment of the Federal Constitutional Court (BVerfG) of 26 February 2020 – 2 BvR 2347/15. Karlsruhe: Bundesverfassungsgericht; 20 Feb 2020.
28. Estonia. Supreme Court judgment in case 1-21-12780. Tallinn: Supreme Court of Estonia; 7 May 2025.
29. A.C. v. Manitoba (Director of Child and Family Services), 2009 SCC 30, [2009] 2 SCR 181. Ottawa: Supreme Court of Canada; 2009.
30. Belgium. Act Concerning Euthanasia. Brussels: Belgian Official Gazette; 28 May 2002.
31. Government of the Netherlands. Termination of Life on Request and Assisted Suicide (Review Procedures) Act. The Hague; 1 Apr 2022.
32. Hurst SA, Mauron A. Assisted suicide and euthanasia in Switzerland: allowing a role for non-physicians. BMJ. 2003;326(7383):271-3.
33. MAID Practice Standards Task Group. Model Practice Standard for Medical Assistance in Dying (MAID). Ottawa: Health Canada; 2023.
34. MAID Practice Standards Task Group. Advice to the Profession: Medical Assistance in Dying (MAiD). Ottawa: Health Canada; 2023.
35. Norberg v Wynrib, [1992] 2 S.C.R. 226.
36. Hopp v Lepp, [1980] 2 SCR 192, 112 DLR (3d) 67.
37. Reibl v Hughes, [1980] 2 S.C.R. 880.
38. Government of Canada. Homicide. Criminal Code, RSC 1985, c C-46, s 222.
39. Nancy B. v Hôtel-Dieu de Québec, [1992] RJQ 789 (Que Sup Ct).
40. Starson v Swayze, 2003 SCC 32, [2003] 1 SCR 722.
41. Roth LH, Meisel A, Lidz CW. Tests of competency to consent to treatment. Am J Psychiatry. 1977;134(3):279-84.
42. Appelbaum PS. Assessment of patients’ competence to consent to treatment. NEJM. 2007;357(18):1834-40.
43. Appel JM. Legal and ethics considerations in capacity evaluation for medical aid in dying. J Am Acad Psychiatry Law. 2024;52(3):311-26.
44. Wiebe E, Kelly M, McMorrow T, Tremblay-Huet S, Hennawy M. Assessment of capacity to give informed consent for medical assistance in dying: a qualitative study of clinicians’ experience. CMAJ Open. 2021;9(2):E358-63.
45. In re Quinlan, 70 NJ 10, 355 A2d 647 (NJ 1976).
46. Cruzan v. Director, Missouri Department of Health, 497 US 261 (1990).
47. Québec. Bill 11, An Act to amend the Act respecting end-of-life care and other legislative provisions. 1st Sess, 43rd Leg, Québec, 2023.
48. Canadian Association of MAiD Assessors and Providers. The Interpretation and Role of ‘Reasonably Foreseeable’ in MAiD Practice. CAMAP; Feb 2022.
49. Picard EI, Robertson GB. Legal Liability of Physicians and Hospitals in Canada. 5th ed. Toronto: Thomson Carswell; 2017.
50. Brassolotto J, Manduca-Barone A, Zurbrigg P. Medical assistance in dying: a review of related Canadian news media texts. J Med Humanit. 2023;44(2):167-86.
51. Wiebe K, Mullin A. Choosing death in unjust conditions: hope, autonomy and harm reduction. J Med Ethics. 2024;50(6):407-12.
52. Christie T, Li M. Medically assisted dying in Canada and unjust social conditions: a response to Wiebe and Mullin. J Med Ethics. 2024;50(6):423-24.
53. Hohfeld WN. Some fundamental legal conceptions as applied in judicial reasoning. Yale Law J. 1913;23:16-59.
54. Department of Justice Canada. Present indicative. Legistics. 29 Aug 2022.
55. Coelho R, Maher J, Gaind KS, Lemmens T. The realities of Medical Assistance in Dying in Canada. Palliat Support Care. 2023;21(5):871-8.
56. Downie J, Schuklenk U. Social determinants of health and slippery slopes in assisted dying debates: lessons from Canada. J Med Ethics. 2021;47(10):662-9.
57. McInerney v MacDonald, [1992] 2 SCR 138.
58. Canadian Medical Protective Association. Medico-Legal Handbook for Physicians in Canada. Version 9.0. Ottawa: CMPA; May 2021 (rev. Oct 2024).
59. Rodriguez v. British Columbia (Attorney General), [1993] 3 S.C.R. 519.
60. Rawls J. A Theory of Justice. Cambridge: Harvard University Press; 1971.
61. Oregon Health Authority. Oregon Death with Dignity Act: 2022 Data Summary. Portland; 2023.
62. Washington State Department of Health. Washington Death with Dignity Act: 2022 Report. Olympia; 2 Jun 2023.
63. California Department of Public Health. California End of Life Option Act: 2022 Data Report. Sacramento; Jul 2023.
64. Health Canada. First Annual Report on Medical Assistance in Dying in Canada 2019. Ottawa; Jul 2020.
65. Health Canada. Second Annual Report on Medical Assistance in Dying in Canada 2020. Ottawa; Jun 2021.
66. Health Canada. Third Annual Report on Medical Assistance in Dying in Canada 2021. Ottawa; Jul 2022.
67. Health Canada. Fourth Annual Report on Medical Assistance in Dying in Canada 2022. Ottawa; Oct 2023.
68. Truchon c Procureur général du Canada, 2019 QCCS 3792.
69. Hawke LD, Bastidas-Bilbao H, Cappe V, et al. Medical assistance in dying for mental illness as a sole underlying medical condition and its relationship to suicide: A qualitative lived experience-engaged study. Can J Psychiatry. 2024;69(5):314-25.
70. Fruhstorfer C, Kelly M, Spiegel L, Baylis PJ, Dembo J, Wiebe E. Patient experiences with requests for medical assistance in dying: Perspectives of those with complex chronic conditions. Can Fam Physician. 2024;70(1):41-7.
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Timothy Christie

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Canadian Journal of Bioethics applies the Creative Commons Attribution 4.0 International License to all its publications. Authors therefore retain copyright of their publication, e.g., they can reuse their publication, link to it on their home page or institutional website, deposit a PDF in a public repository. However, the authors allow anyone to download, reuse, reprint, distribute, and/or copy their publication, so long as the original authors and source are cited.














_smaller.png)